It Takes a Village: Collaboration in a Healthy Revenue Cycle
You are seeking new strategies to improve your company’s current revenue cycle and reduce obstacles. But how could the way you approach your revenue cycle make a difference?
One of the most impactful and recurring procedures in healthcare organizations is the revenue cycle. A healthy revenue cycle depends on all teams in a healthcare organization. It is a series of systems, operational services, and teams that contribute to the processing and collection of payment for services from all responsible parties. It starts with the first patient contact and continues until the patient is no longer receiving care. Typically, we find that for a CFO, these challenges may include: access to the proper metrics, unclear accountability across departments, managing up, down, and sideways, healthcare systems of record and best practices, including vendor management, month-end reconciliation, and payment model forecasting.
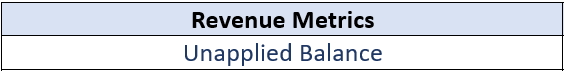
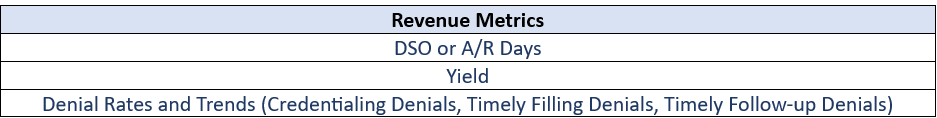
A healthy revenue cycle utilizes a systematic approach. We advocate for a strong operational approach, co-ownership, continuous process improvement, prioritization, delegation, and capacity planning. The revenue cycle can be broken down into five stages, which include patient registration, service documentation, payment posting, and accounts receivable strategy. We offer a definition and objective, as well as operational and financial metrics to monitor each stage.
Connecting the components of the revenue cycle means building deep connections between the teams. Tying together rewards and outcomes so that each individual shows up with a clear understanding of how they can influence organizational objectives and positively impact the patients they serve.
Complete Revenue Cycle
Patient Registration
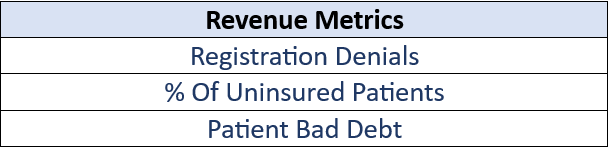
Patient registration focuses on: who we are serving, and who is accountable for paying for that service. In this stage, the front office creates an accurate representation of demographics, including insurance setup. Insurance setup ensures accurate billing and allows an organization to identify patients in need of insurance and financial assistance.
Service Documentation
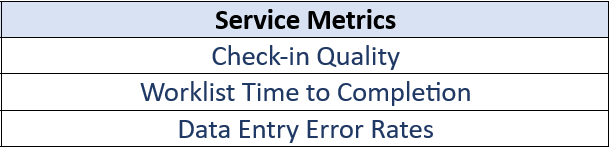
Service documentation focuses on: what service specifically did we provide? The purpose of this step is to ensure continuity of care regarding diagnosis, treatment, and management of orders and referrals.
Coding
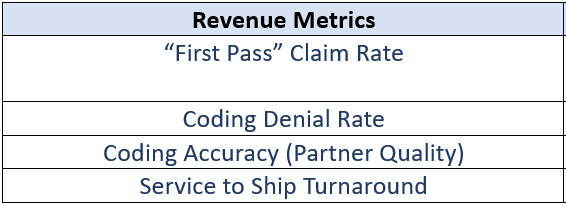
The purpose of coding is to translate service documentation, diagnosis, and treatment to a universal and standardized code set (CPT and ICD10) for billing/reimbursement and epidemiological study.
Payment Posting
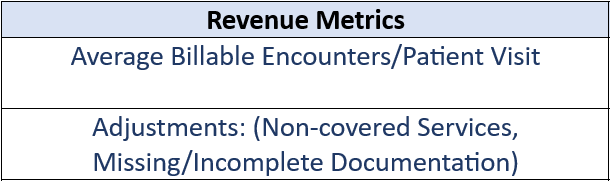
All Transactions matter. The purpose of payment posting is to post all payments, adjustments, and denials to each voucher in the practice management system of record.
Accounts Receivable Strategy (A/R)
The primary objective of this stage is to ensure that what is owed is collected. A/R strategy includes utilizing data, prioritizing effort, leveraging system solutions, and utilizing partners for a strong yield.
Each phase in the revenue cycle depends on strong processes and data from the previous stage. In our experience, a weakness in any area—whether the beginning, middle, or end of a cycle—will impact an organization’s ability to collect all that is owed as quickly and efficiently as possible. It will cost the organization in terms of uncollected dollars, or increases in the cost to collect, taking funds that could otherwise be invested in the providers and patients.
By taking a proactive, end-to-end approach to revenue cycle management, organizations can close the gaps, strengthen financial performance, and ultimately reinvest more into patient care and provider support. The sooner inefficiencies are identified and addressed, the stronger and more resilient the entire system becomes.
Thanks for reading—we appreciate your time and interest in building stronger and more sustainable healthcare operations.